A Primer on Medical Directives for Physician Assistants
PAs in Ontario practice with medical directives. Medical directives are a written document that serve as indirect orders from a physician to a health care provider. Medical directives can be carried out when specific conditions are met.
Each province’s college has different policies surrounding the delegation of controlled acts. What is presented here is based on the Ontario experience.
How do PAs Practice in Ontario?
PAs are autonomous, but dependent practitioners. By nature Physician Assistants are not independent practitioners, we work under the supervision of physicians. As outlined by OHA, the definition of “supervision” varies – this can be direct (direct observation) or indirect (physician offsite, but accessible via phone or electronic means).
At the beginning of a PA’s employment, it may be more appropriate to have “direct” supervision, however as the PA/MD relationship develops, and the PA builds knowledge, competency and skills in their area of practice, the supervision may transition to “indirect”.
In Ontario, Physician Assistants practice through the Regulated Health Professions Act (RHPA), which outlines controlled medical procedures that can be delegated to PAs by physician orders – written, verbal or medical directives. This differs from province to province, so check each province’s college website to determine how PAs can practice in your jurisdiction.
What are Medical Directives?
According to the College of Physician and Surgeons of Ontario (CPSO),
“Medical directives are written orders by physicians…. to other health care providers that pertain to any patient who meets the criteria set out in the medical directive. When the directive calls for acts that will require delegation. It provides authority to carry out the treatments, procedures or other interventions that are specified int he directive, provided that certain conditions and circumstances exist.”
Medical Directives serve as an “authorizing mechanism” to allow Physician Assistants to performed controlled acts:
There are 14 controlled acts as listed by the College of Physician Assistants in Ontario. PAs may be delegated 12 out of the 14 acts may be delegated via direct order.
As an unregulated health professional, direct orders or medical directives are required for PAs to legally perform delegated controlled acts and provide patient care.
Although medical directives can be cumbersome and challenging to create, they do improve the efficiency of PA practice and allow for some practice autonomy as they avoid the need for constant verbal orders from supervising physicians.
Medical directives should be developed to allow the PA to practice at the top of their scope of practice, and be implemented as soon as possible, as it requires approval from different levels of hospital or clinic administrations and decision makers. These changes may reflect changes in staff/supervising physicians and expansion of PA knowledge and skills.
Proper medical documentation is essential for liability purposes.
In other words, the medical directive allows a supervising physician to delegate duties to another person without requiring the physician’s physical presence. CPSO has a list of 14 controlled acts that can be delegated. The medical directive expands on these delegated tasks to outline certain conditions under which PAs can perform those delegated tasks.
Although a very simplistic example, think of medical directives like a “Protocol” with many “If, then” statements. “If patients presents with X, PA is to perform Y“.
X being condition specific, or certain presentations, or a list of indications. It can also be related to preventative care (e.g. when patient is due for a well baby exam).
Y being assessment (history & physical exams), ordering or performing diagnostic or therapeutic procedures and prescription of medications . Contraindications included.
Keeping Medical Directives Updated
Medical directives are living documents, they should be updated frequently (at most every 3-4 years) as guidelines change.
Include References in Your Medical Directives which may include a “See Canadian Diabetes Association Clinical Practice Guidelines for Screening & Diagnosis of Diabetes” with a link to the website. You may include the actual guidelines as an Appendix at the end of the medical directive, or built right into the medical directives, however this does require a lot of upkeep when the guidelines update.
“ry to keep your directives broad instead of specific” i.e. instead of listing individual medications list classes or medications or group together by disease processes.
An example would be to say you can prescribe Sulfonylureas (class of medication) instead of Diamicron (specific medication) or even better, all antihypoglyemic medications (by disease process). This ensures directives do not need to be updated every time a new medication comes on the market.”
How Medical Directives serve as a Mechanism for Physician Orders
There are three methods to take orders from physicians:
Verbal Direct Order – in person or over the phone. Requires presence of a physician. This takes place after the PA has interacted with a patient.
Written Direct Order – having the physician spell out/write out orders and sign off. This takes place after the PA has interacted with a patient.
Medical Directives – PAs are able to implement an already-agreed-upon list of frequently delegated tasks under certain circumstances. This takes place in advance of the PA interacting with a patient.
In all cases, how the order was implemented (and method – verbal, written, medical directives) should be documented in the patient’s chart.
Medical directives allow PAs to perform various delegated acts under the supervision of a physician. The physician does not necessarily need to be present for the PA to perform these delegated tasks that have been outlined in the medical directive. Medical directives allow PAs to function more efficiently, especially in settings with indirect physician supervision.
It can be quite cumbersome to require your supervising physicians to give you verbal or written orders or to chase after physicians (around a hospital, or smaller practice) for routine ordering of imaging, lab tests, and prescription of routine medications (narcotics/controlled substances fall out of this scope). Time is spent instead on patient care.
If there is a controlled act, e.g. an investigation you would like to order, a medication that you would like to prescribe (such as a narcotic/controlled substance), or an intervention you would like to implement that falls outside of the medical directives, this is where you would require a direct order (e.g. written order) from the physician.
What do Medical Directives look like?
Medical directives can be very broad or specific. They will be formatted to best suit the practice setting – Emergency Medicine Medical Directives will look very different from Medical Directives in a Family Medicine Setting and are often institution-specific.
Some practice settings have already prepared Medical Directives, other places require the PA to develop the medical directives, which can be an enormous (but not impossible!) undertaking.
Components of a Medical Directive
History and Physical Examination (should encompass or mention)
Medical Documentation
Ordering lab investigations
Ordering Investigations:
X-rays
ECGs
Ultrasound
Echocardiogram
CT
MRI
Prescribing Medications: Some allow PAs to prescribe from drug formularies that are small, and some are larger formularies.
An example of a general statement in a medical directive that does not list any medications, but instead say, “PA may order medications, but this does not include narcotics or benzodiazepines).
Performing Procedures
Sutures
Casting and Splinting
PAP smear
Surgical Assist
Ordering IV Fluids
Referrals:
Referral to allied health professionals (e.g. referring to a dietitian, massage therapy, physiotherapy, occupational therapy assessment).
Referral to other MD
May sign CCAC referral
Verbal Orders – More recently some medical directives have included the ability to transcribe verbal order sin chart. Recently CNO resource. Check your institution policy.
Extra Points to Include in the Medical Directive
Indications and Contraindications to Implementing the Medical Directive should be included
Some directives are very specific (e.g. in case of GI bleed, medication should not be prescribed) or very vague (e.g. in the case of medical directove for history taking, indication is any patient admitted in X hospital, under X service, with X physician).
Some directives advise to refer to external resources (e.g. Clinical Practice Guidelines or Rx Files) for indications and contraindications of medications and procedures.
Certification/Education Requirements
There should be a statement defining the Certification and Education requirements of Physician Assistants that are to implement the medical directive. This may include:
“Physician Assistant passed the PACCC, or be PA-C
“Physician Assistant must have liability insurance”
Optional: Additional Competency Assessment
If a PA is performing a delegated controlled act, they must be capable of performing it safely and competently. Without regulation in Ontario, there is no official process for determining an individual’s competence other than the PA Entry to Exam. The medical directives may have a component of “competency assessment”.
How to document implementation of a Medical Directive
The most common place I have seen medical directives directly referenced is when PAs write prescriptions for medications or are ordering investigations. Here is a few examples how the implementation of a medical directives is documented:
Medical Directives & Medical Documentation – Whenever you perform a delegated act outlined in the medical directive, there should be a reference to it when you are documenting your patient encounter.
Medical directives reference can be specific per encounter
e.g. “Counseled patient on medication use and compliance, self-monitoring of blood glucose levels, smoking cessation, alcohol consumption, exercise and diet as per medical directive #12c”
e.g. “After explaining risks and benefits, and obtaining informed consent, 80 mg of Depo-Medrol along with 4 cc of 2% Xylocaine without Epinephrine was injected into the right knee using sterile technique, no complications. Intervention performed as per medical directive #12d”
Or it can be all-encompassing: At the end of the documentation capturing the patient care (Consult note, follow-up note, progress note, SOAP note, etc.) you can include this when you sign off your name:
John Smith, CCPA as per PA Medical Directive #6
Medical Directives & Ordering Investigations – Ensure local imaging facilities have a copy of the medical directives. When signing at the bottom, sign your name, designation, medical directive reference, the supervising physician's name and their CPSO number.
e.g. John Smith, CCPA, as per medical directive #2a for Dr. Jane Appleby, CPSO # 86070. Clinic: Peach Tree CHC, 123 Long Street, Toronto, ON M3U 5Y5″
Medical Directives & Prescription Medications – Ensure the pharmacies that your patients go to (whether hospital/inhouse pharmacy or community pharmacy) have a copy of your medical directives. Take it a step further and introduce yourself personally to the pharmacist with a copy of a photo resume, medical directives (with sections marked/highlighted as relevant to the pharmacists), a copy of the Ontario College of Pharmacists Bulletin on PAs (its page 13 and 14), clinic address, at the bottom of the prescription write e.g. John Smith, CCPA “as per medical directive #1a”, your supervising physician name and their CPSO number.
e.g. John Smith, CCPA, as per medical directive #2a for Dr. Jane Appleby, CPSO # 86070. Clinic: Peach Tree CHC, 123 Long Street, Toronto, ON M3U 5Y5″
Ensuring competence to perform a directive
Being able to implement a medical directive (and also being able to delegate a controlled act) requires a few things:
The supervising physician can only delegate an act that they themselves are competent at, and are within the scope/area of medicine that they practice. They cannot delegate acts that fall outside of this.
CPSO outlines that the delegate (PA) should be evaluated by supervising physician to ensure the PA has the appropriate knowledge, skill and judgement to perform the act just as well as the supervising physician. How this can be evaluated is a competency checklist. For instance, your supervising physician (or designee) can observe you do a certain delegated act (e.g. performing a lumbar puncture) 10 times, at certain time points. This can be implemented directly into the medical directives. And this can be checked annually, bi-annually or at whatever frequency the practice deems fit.
You can decline the delegated act for any reason, you cannot be forced by the delegating physician to perform the act.
More information can be found on CPSO’s Delegation of Controlled Acts Page.
Examples of Medical Directives
Database of PA Medical Directives
The best place to find medical directives for PAs are on the CAPA Members Site under “Resources” > Medical Directives. This database includes several examples of Medical Directives from various areas of medicine including Family Medicine, Hospital (Internal Medicine, General Surgery, Emergency Medicine and Orthopaedic Surgery) and Specialty Medical Directives (Endocrinology, Mental Health, and Oncology).
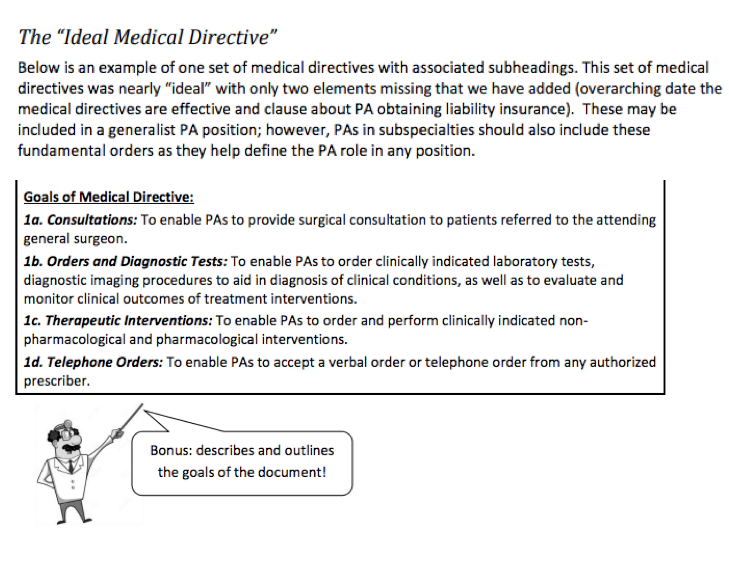
CAPA members Natalie Dies & Ken Krosby also have put together a generic “Ideal Medical Directives Template“.
Medical Directives Online
If you google “Physician Assistants Medical Directives” there are a few clinics and departments that have PDFs of their medical directives online:
Family Medicine – Hamilton Family Health Team: List of Medical Directives [example of specific medical directives]
Family Medicine – Thames Family Health Team: List of Medical Directives
Family Medicine – Marathon Family Health Team Medical Directives [example or broad medical directives]
Emergency Medicine – ED Medical Directive Templates from OHA
Emergency Medicine – Lakeridge Health Team Medical Directives
Emergency Medicine (Asthma) – Emergency Department Adult Asthma Medical Directive
INR Clinic – King West: Medical Directives for INR Clinic
Tips on Creating Medical Directives
Start working on your medical directives as early as possible, as time of creation to full implementation maybe 4-6 months or more
Educate your supervising physicians on medical directives and how they will be implemented.
Approach health care team members (RN, allied health, administrators) about supervising physicians, and offer to be present at meetings where your medical directives will be discussed
Provide examples of other medical directives implemented in similar areas of practice
Contact CAPA if you are having any difficulty with any aspect of your medical directives. They are an excellent resource.
Respect and understand that supervising physician and administrators may be hesitant in implementing them
PA Medical Directives and working with Nurses
Through a medical directive, the PA acts as “vehicle” of delegation. Therefore the nurse and PA are co-implementing the order. There may be a statement or section on the medical directive document that clarifies this piece.
Do All PAs need Medical Directives?
This answer is very institution dependent.
Many Community Health Centres (CHCs), Family Health Teams (FHTs) and hospitals have medical directives in place as part of their policy. In instances where PAs practice with a lot of indirect physician supervision medical directives can be extremely helpful. (e.g. wards, inpatient units, hospital settings, or at a family practice setting where you have your own roster of patients),
In more direct supervision settings, medical directives may not be necessary.